Focus lung tuberculosis.
The focus lung tuberculosis is referred to manifestation of secondary tuberculosis, is the initial form of the lung tuberculosis of the adult. To this form concern: acute, or fine focus tuberculosis and fibrotic focus tuberculosis, long-standing, with the size of focus formation no more than 1 cm in a diameter.
Acute focus lung tuberculosis morphologicaly is shown by development of endo- and peri-bronchitis of the fine apical branches of the 1-st and 2-nd order of the segmental bronchi with subsequent caseous necrosis in the bronchi walls. The involving in the specific process of the near by air-cells results in formation of the caseous acinus or lobular bronchial pneumonia. During the long period, the process in the lungs is limited to territory of an acinus or lobule. At the tendency to progressing, around of the originally arisen focuses new ones appear, developing by contact within the limits of the same lung segment. The lympostasis develops in the lymphatic passes, fibrotic tissue layers, peribronchial and perivascular tissues, passing to the lungs roots.
The typical way of the lung focus tuberculosis progressing is bronchogenic, with development of the new bronchial pneumonic focuses. Damage of the lymphatic nodes are not characteristic. At favorable course the bronchopneumonic focuses are exposed to encapsulation, calcification, fibrosis or hyalinoses. The reinfected focuses (“reinfects”) have latent development at the fibrotic focus lung tuberculosis, but under adverse conditions, their aggravation possible with exudative reactions and growth of a zone of necrosis. At the defeat of the bronchial tree with MBT expectoration a destructive form (cavitary) of the lung tuberculosis develop. At the tubercular process reverse quite often diffuse sclerosis develops of the top segments.
Infiltrative-pneumonic lung tuberculosis.
The infiltrative lung tuberculosis is known for a long time. T.H. Laenec [1781-1926], on the basis of the section data has described it as jelatinoid pneumonia. The infiltration develops as a result of an aggravation of encapsulated focuses, which can be not only in lungs, but also in intrathoracic lymphatic nodes. When an infiltrative focus develops in the unaltered tissue, then around fresh tubercular focus or fused several focuses centers perifocal inflammation develops. Infiltrative lung tuberculosis is characterized by presence in lungs inflammative changes, mainly of exudative character with caseouse necrosis and with presence or absence of lung tissue destruction. Aetiology of infiltrative lung tuberculosis can be of various origin. Among one group of patients, infiltrative focuses are developed as a result of bronchogenic dissemination of bacilli to healthy pulmonary tissue and from inflamed latent apical focuses. In other group of patients infiltrations represent the perifocal inflammation of small infiltrative focuses of older origin, which consequently radiographically difficult to be determined.
The pathological-anatomical picture of the infiltrative-pneumonic lung tuberculosis is characterized by presence one or several fine focuses of cheesy necrosis, with different time duration with a zone of perifocal inflammation, which volume exceeds their sizes in several times. The character of the exudate is various at this form: serous, serous-fibrinous, sometimes as desquamative alveolitis, gelatinous infiltration. According to extent, the process can be limited by lobule, but can occupy all lobe of a lung. Proliferative reaction comes to an end by development of a connective tissue, turning to itself interstitially indurative fibroid fields.
Outcomes of the infiltrative-pneumonic lung tuberculosis:
- complete resorption of the perifocal zone or carnification of the damaged focus with encapsulation and calcification (transition to fibrotic focus form);
- caseation of the perifocal zone of inflammation, joining of disintegration, sequestration and transition into the acute caseous pneumonia or cavernous lung tuberculosis;
- at predisposition of infiltration to development of caseous necrosis the infiltration is exposed to complete or partial disintegration. As a result of caseous mass discharge the pneumogenic cavity is formed which size depends on a volume of infiltrative pneumonic focus and necrosis.
Caseous pneumonia.
The caseous pneumonia arises more often in result of progression the infiltrative-pneumonic lung tuberculosis, but can aggravate the development of any form of lung tuberculosis. The basic morphological attribute of the caseous pneumonia is prevalence of caseous changes above unspecific perifocal. Depending on the size of the lung damaged volume distinguish the following caseous pneumonia:
- acinous;
- lobular confluent;
- segmental;
- lobar caseous.
At caseous pneumonia progressing the polycavernous lung tuberculosis develops.
Lung tuberculoma.
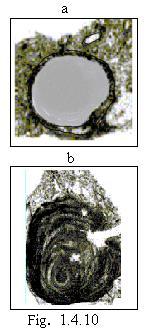 The lung tuberculoma has the distinctive original clinical and anatomical display of secondary form of the lung tuberculosis. It is characterized by the development of the dense caseous focus (some time several focuses) in lungs, of the rounded form, sharply outlined from surrounding tissue by fibrotic capsule. (Рис./Fig. 1.4.10.)
The lung tuberculoma has the distinctive original clinical and anatomical display of secondary form of the lung tuberculosis. It is characterized by the development of the dense caseous focus (some time several focuses) in lungs, of the rounded form, sharply outlined from surrounding tissue by fibrotic capsule. (Рис./Fig. 1.4.10.)
The source of tuberculoma formation basically two forms of lung tuberculosis are served: infiltrative-pneumonic and focus. Besides tuberculoma could be formed from cavernous lung tuberculosis by means of filling of cavity with caseous masses. The filled cavities refer to tuberculoma only conditionally, as the filling of a cavity occurs mechanically, while tuberculoma — it is an original phenomenon in lung tissue.
Tuberculema can be solitary (homogeneous (a) and of layered structure seeing on a section (b), multiple and conglomerative, consisting from group of the focuses with common capsule. (See Fig. 1.4.10.)
The following kinds of the tuberculoma are marked out:
- the infiltrative-pneumonic tuberculoma represents encapsulated rather fresh focus of caseous pneumonia;
- a caseoma regarded as the following stage in evolution of delimited cheesy focus (melting, condensation, calcification, dissolution);
- the filled cavity – psevdo-tuberculoma.
Variants of the tuberculema aggravation;
- development of the perifocal inflammation;
- cavitation – discharge of the caseous masses from a cavity, through draining bronchus.
Cavernous lung tuberculosis.
Cavernous tuberculosis is characteristic by presence of a thin-walled cavity, without perifocal inflammation, with solitary focuses in surrounding tissue.
 Cavernous lung tuberculosis arise from:
Cavernous lung tuberculosis arise from:
- melting of the caseous bronchopneumonia, from the tuberculous infiltrative-pneumonic focus in lungs (the pneumogenic acute cavity);
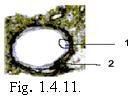
- from the focus with a capsule in past (tuberculoma) Fig. 1.4.11. Regions of not tear away caseous necrosis remain on an internal surface of such cavities.
Complications of the cavernous tuberculosis.
For the acute cavernous lung tuberculosis bronchogenic way of progressing is typical. Concerning complications of the cavernous tuberculosis it is necessary to note an opportunity of the profuse hemorrhage. The acute cavernous tuberculosis at the further development converts into the fibrotic-cavernous one.
Fibrotic-cavernous lung tuberculosis.
Fibrotic-cavernous lung tuberculosis develops from any progressing form of lung tuberculosis with formation of a cavity, in which the wall is expressed by fibrotic component. Certainly, at far advanced fibrous-cavernous lung tuberculosis it is not easy to define what process was its source and that has served as the reason for its development. Progression of the fibrotic-cavernous lung tuberculosis developed by contact way and along bronchi in direction from the top of the lungs to their base. The defeat of the bronchial tree reveal in all cases of fibrotic-cavernous lung tuberculosis (Fig. 1.4.12.).

The damage extent in lungs can be various. The process could be unilateral and bilateral with presence of one or multiple cavities. For fibrotic-cavernous tuberculosis the focuses of bronchogenic is repeated in various times dissemination are characteristic. As a rule, the cavity drainage bronchus is damaged. Other morphological changes develop also in lungs such as pneumosclerosis, emphysema bronchoectasia.
Cirrhotic lung tuberculosis.
 The lung cirrhosis represents involution phase of development disseminated or fibrous-cavernous lung tuberculosis, arising because of growth lung connecting tissue. Massive sclerosis develops at infiltrative pneumonic carnification processes, pulmonary fibrosis as a result of long developing atelectasis. At development of cirrhotic lung tuberculosis, along with massive, overgrowth of the connecting tissue of diffuse character, deformation of a lung tissue and bronchectasis development take place. The cavities are absent or look like narrow slit-like cavities. At significant volume of the sclerotic changes hypertension of a small circle blood circulation, cor pulmonale and lung-heart insufficiency develop. To the basic complications concern also the amyloidosis of internal organs and tromboembolism of the lung artery (Fig. 1.4.13.).
The lung cirrhosis represents involution phase of development disseminated or fibrous-cavernous lung tuberculosis, arising because of growth lung connecting tissue. Massive sclerosis develops at infiltrative pneumonic carnification processes, pulmonary fibrosis as a result of long developing atelectasis. At development of cirrhotic lung tuberculosis, along with massive, overgrowth of the connecting tissue of diffuse character, deformation of a lung tissue and bronchectasis development take place. The cavities are absent or look like narrow slit-like cavities. At significant volume of the sclerotic changes hypertension of a small circle blood circulation, cor pulmonale and lung-heart insufficiency develop. To the basic complications concern also the amyloidosis of internal organs and tromboembolism of the lung artery (Fig. 1.4.13.).
At involution of infiltration or fibrous-cavernous tuberculosis the cirrhosis could be unilateral and bilateral, according to extent of tubercular process. The diffuse net-like sclerosis is most often met in cases of hematogenic spreading tuberculosis. The vicarious emphysema accompany cirrhotic process in lungs, which develops in the undamaged parts of the lungs. Replacement of lung normal tissue by scarring material, deformation of bronchial lumen damage bronchial function. This process results in accumulation of biological fluid in bronchi, where MBT grow intensively and secondary inflammative processes develop. The deformation of bronchi results in development bronchectasis Deformation, narrowing and obliteration of vessels develop under influence of pneumosclerosis, formation of vascular ectasia.
The structural changes of bronchi, reduction of respiratory excursions because of pleural knitting and emphysema result in infringement of breath function. The mass destruction of alveoli and lung capillaries damage alveoli gas exchange. Hypoxia and hypoxemia develop. The respiratory insufficiency is compensated by right heart muscle hypertrophy. When heart compensatory abilities are diminishing, to respiratory insufficiency joins heart insufficiency and syndrome “Cor pulmonale” develops. In later stages of cirrhosis development to right heart insufficiency the insufficiency of the left ventricle joins. One of the basic reasons of death of the patients with cirrhotic lung tuberculosis is the insufficiency of blood circulation. Right ventricle type decompensation of the heart.
Tubercular pleurisy.
The pleurisy, is the inflammation of pleura. Two basic forms of pleurisy are distinguished: dry, or fibrinous (pleuritis sicca, fibrinosa), and exudative (pleuritis exudativa). At tuberculosis the pleura is involved in the process of inflammation at infection penetration in it by contact way, through the lymph or the blood. Involving of pleura in various pathological processes is caused by close anatomic topographical connections of visceral and parietal pleura with lung tissue, intrathoracic lymphatic nodes. The pleura, having barrier function, reacts on various pathophysiological changes in a body, therefore inflammative or allergic processes develop in it.
Exudative inflammative reaction of the pleura is connected with increased permeability of the blood and lymphatic capillaries of the lung cortical layer and pleura itself. These capillaries making way for a liquid part of blood in intra tissue fissures, superficial layers of pleura and there from, owing to negative pressure, into pleural cavity.
Lymphagenic pleurisy.
The tubercular infection can affect subpleural lymphatic nodes. Mycobacterium tuberculosis accumulate in subpleural lymphatic nodes partially bricked up and eliminated. Partially MBT, keeping their virulence, are distributed along lymphatic passes and cause subpleural cortical lymphangiitis or the exudative pleurisy.
Hematogenic pleurisy.
It is possible hematogenic spreading of MBT into the pleural cavity, with development on pleura tubercles. The initial focus is the active tubercular process, in mediastinum lymphatic nodes. The contact way of MBT dissemination arises at active tuberculosis of lymphatic mediastinum nodes, with defeat of visceral pleura.
Acute pleurisy.
The serous pleurisy is seldom observed. At the fibrinous pleurisy (dry pleurisy) on the pleura at first gentle layer occurs, of fibrinous structure which could be easily removed. Further the fibrinous pellicleof yellowish or yellowish-gray color is formed.
Purulent pleurisy (empyema) seldom from the very beginning arises as purulent, more often develops after serous-fibrinous inflammation of the pleura. The process usually happens unilateral and mainly settles down in basal or posterior part of the pleural cavity. The purulent pleurisy is observed at bursting out of caseous masses from lung into the pleural cavity, broncho-pleural fistulas and etc.
Hemorrhagic pleurisy is accompanied by penetration of an exudates containing a significant impurity of erythrocytes into pleural cavity.
Outcome of acute pleurisy.
Serous exudates can completely dissolve.
In overwhelming majority of cases the fibrinous exudates dissolves only partially, and basically is subjected to transformation, that leads to development of commissural joints, fibrotic thickening of the pleura, to obliteration of the pleural cavities.
Purulent exudates seldom is exposed to complete dissolution, more often the encapsulation of the inflammative effusion is developed. The inflammative process at pleural empyema can pass on interstitial lung tissues (purulent pneumonia).
Chronic pleurisy.
More often chronic course of the pleurisy is observed at pleural empyema. In these cases exudates is condensed, dissociate, turns in easily soiled, cheesy mass or thin gruel with presence of cholesterol crystals; the microorganisms can disappear. The pleural membranes are considerably thickened, dense, sometimes with focus petrification and even with the ossification. The significant sediments of calcified masses is especially typical for tubercular empyema. The pleural empyema can lead to purulent – resorption fever, sepsis, exhaustion, amyloidosis of internal organs. Sometimes long, chronic current is observed at serous-fibrotic and fibrotic pleurisy. At the acute and chronic pleurisies the significant exudates accumulation in the pleural cavity causes displacement of the mediastinum organs to the opposite side.