Separation of two consecutive periods of tuberculosis development – primary and secondary – reflects pathomorphological and clinical picture of the disease. Post primary (secondary) tuberculosis – this definition is used for tuberculosis, which developed in organism with old post primary lesions, which had been partially healed. Occurrence and development of secondary tuberculosis can rise in two ways:
- reactivation of the residual post primary focuses (partially calcified lymphatic nodes)-endogenous super infection;
- super infection (reinfection) – repeated tuberculosis infection – exogenous super infection.
Secondary tuberculosis (in most cases – 90%) — is lung tuberculosis.
The initial tubercular changes of a secondary period in lungs quite often are found out at fluorography or on X-ray, made during preventive checkup without any complaints of the patients. This tendency is one of the indirect proofs that the patient does not feel the illness, as it developed asymptomatically. In such cases on X-ray tubercular affections look like the medium-sized focuses in lungs or in the other organs. However, in lungs they meet more often and are much more accessible for clinical and X-ray diagnostics.
The distribution of infection often goes through bronchial way at secondary tuberculosis progression.
For the bronchogenic forms of disseminated lung tuberculosis it is characteristic the presence of the initial focus in lung or in intrathoracic lymphatic nodes at absence of infiltrative focus with disintegration or cavernous lung tuberculosis. At infiltrative process with disintegration or cavernous tuberculosis the bronchogenic dissemination will be a phase progression of the process. The most important event that determines if the patient, especially the adult patient, will have significant clinical tuberculosis is the softening and liquefaction of the caseous necrotic material. During liquefaction, there is a massive increase in the number of bacilli which (for the first time) grow extracellularly. Liquefaction tends to occur in organs having not compact structure like the lungs have, serous surfaces of organ’s cavities, or canalicular organs like the kidneys. Such process occurs rarely in solid organs like the liver. Liquefaction can occur in local areas of the caseous mass and to expand to other parts.
Evolution of secondary tuberculosis.
Schematic appearances of lesions progression in an adult (Fig. 1.4.9.).
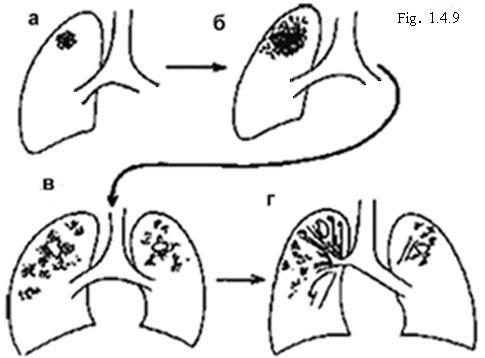
- Primary lung lesion in an adult. It is often in the upper part of the lung. The lesion in the hilar lymph node usually absent (though sometimes – among Africans, Asians or patients with HTV infection – the nodes may be greatly enlarged). The lung and lymph node lesions often heal and may later calcify.
- At progression of secondary tuberculosis there may be:
Gradual enlargement of the lung lesion, - Caseation (necrosis) of the lesion. Liquefied caseous material may be coughed up. This results in a cavity. Spread of TB from the cavity to produce further lesions in the same and in the opposite lung (with a further cavity developing in that lung),
- After a year or two of effective treatment (if the patient survives) fibrosis (scarring), cavities develops which pulls up the hilum and the trachea to the side of biggest damage.
Calcification is starting in most early developed apical lesions. But the cavities can be still open. This type of ‘chronic survivor’ is a major source of infection. The presence in lungs of characteristic pathomorphological manifestations are used as a basis to classify secondary lung tuberculosis on the forms:
- focus lung tuberculosis;
- infiltrative-pneumonic lung tuberculosis;
- caseous pneumonia;
- lung tuberculoma;
- cavernous lung tuberculosis;
- fibrotic-cavernous lung tuberculosis;
- cirrhotic lung tuberculosis;
- tubercular pleurisy.